9.1 Human gas exchange
- Describe the features of gas exchange surfaces in humans, limited to: large surface area, thin surface,good blood and air supply?
Features of Gas Exchange Surfaces in Humans
Gas exchange in humans occurs primarily in the alveoli of the lungs.
These tiny, balloon-like structures are specifically designed to optimize the diffusion of oxygen into the blood and carbon dioxide out of the blood.
Key Features:
- Large Surface Area:
- The alveoli are incredibly numerous, providing a vast surface area for gas exchange.
- This maximizes the contact between the blood and the air, allowing for efficient diffusion.
- Thin Surface:
- The alveolar walls are extremely thin, often just one cell layer thick. This shortens the diffusion distance, enabling oxygen and carbon dioxide to move quickly between the air and the blood.
- Good Blood and Air Supply:
- The alveoli are closely surrounded by a network of capillaries, ensuring a constant supply of oxygen-depleted blood.
- At the same time, the respiratory system delivers a continuous flow of air to the alveoli, maintaining a high concentration of oxygen.
- State the percentages of the gases in atmospheric air?
The primary gases in atmospheric air and their approximate percentages are:
- Nitrogen (N2): 78%
- Oxygen (O2): 21%
- Argon (Ar): 0.93%
- Carbon dioxide (CO2): 0.04%
Other gases, such as neon, helium, methane, krypton, and hydrogen, are present in trace amounts.

- Investigate and explain the differences between inspired and expired air?
| Inspired air | Expired air |
| · The air that is taken inside the body through the nostrils during inhalation is called the inspired air. | · The air that is given out from the lungs during the process of exhalation is called the expired air. |
| · The inspired air is rich in oxygen. | · The expired air is rich in carbon dioxide. |
| · The temperature of the inspired air is variable. | · The temperature of the expired air is the same as that of the body, i.e. 37∘C. |
| · It contains less water vapour. | · It contains more water vapour. |
- Identify, on diagrams and images, the larynx, trachea, lungs, bronchi, bronchioles, alveoli and associated
Capillaries
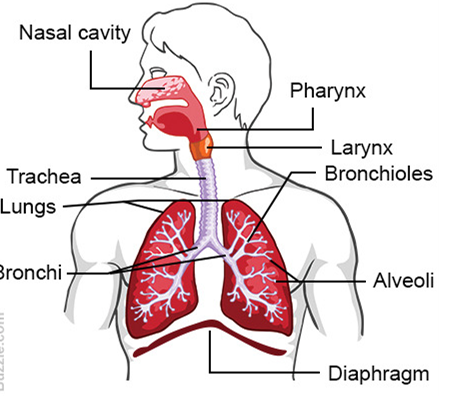
- Larynx (Voice Box):
Located at the top of the trachea, it contains vocal cords that vibrate to produce sound.
- Trachea (Windpipe):
A tube that connects the larynx to the bronchi. It is supported by rings of cartilage to prevent it from collapsing.
- Lungs:
A pair of large, spongy organs located on either side of the chest. They are responsible for the exchange of oxygen and carbon dioxide.
- Bronchi:
The trachea divides into two bronchi, one for each lung.
- Bronchioles:
The bronchi branch into smaller and smaller tubes called bronchioles.
- Alveoli:
Tiny, balloon-like sacs at the end of the bronchioles where gas exchange occurs.
- Capillaries:
A network of tiny blood vessels that surround the alveoli. They carry oxygen-depleted blood to the lungs and oxygen-rich blood away from the lungs.
A more detailed view of the alveoli and capillaries:
- State the characteristics of, and describe the role of, the exchange surface of the alveoli in gas exchange?
The alveoli are the primary sites of gas exchange in the lungs. Their unique characteristics are optimized for efficient diffusion of oxygen into the blood and carbon dioxide out of the blood.
Characteristics:
- Large Surface Area:
The alveoli are incredibly numerous, providing a vast surface area for gas exchange. This maximizes the contact between the blood and the air, allowing for efficient diffusion.
- Thin Walls:
The alveolar walls are extremely thin, often just one cell layer thick. This shortens the diffusion distance, enabling oxygen and carbon dioxide to move quickly between the air and the blood.
- Close Proximity to Capillaries:
The alveoli are closely surrounded by a network of capillaries, ensuring a constant supply of oxygen-depleted blood and a continuous removal of carbon dioxide-laden blood.
Role in exchange
- Oxygen Diffusion:
Oxygen from the inhaled air diffuses across the thin alveolar walls into the nearby capillaries. This occurs because the oxygen concentration in the alveoli is higher than in the blood.
- Carbon Dioxide Diffusion:
Carbon dioxide, a waste product of cellular respiration, diffuses from the blood in the capillaries across the alveolar walls into the alveoli, where it is exhaled.


- Identify, on diagrams and images, the ribs, internal and external intercostal muscles and the diaphragm?
- Ribs:
A series of curved bones that form the framework of the chest cavity.
- Internal Intercostal Muscles:
Muscles located between the ribs. They help to pull the ribs downwards and inwards during exhalation.
- External Intercostal Muscles:
Muscles located between the ribs. They help to lift the ribs upwards and outwards during inhalation.
- Diaphragm:
A dome-shaped muscle that separates the chest cavity from the abdominal cavity. It plays a crucial role in breathing.
- Explain the role of the ribs, the internal and external intercostal muscles and the diaphragm in producing
volume and pressure changes in the thorax, causing the movement of air into and out of the lungs
(breathing)?
The Mechanics of Breathing
Breathing involves the rhythmic movement of air into and out of the lungs. This movement is primarily driven by changes in volume and pressure within the thoracic cavity. The ribs, intercostal muscles, and diaphragm play crucial roles in producing these changes.
The Role of the Ribs and Intercostal Muscles:
- Inhalation:
The external intercostal muscles contract, lifting the ribs upwards and outwards. This expands the thoracic cavity, increasing its volume. As the volume increases, the pressure within the cavity decreases, creating a vacuum that draws air into the lungs.
- Exhalation:
The internal intercostal muscles contract, pulling the ribs downwards and inwards. This decreases the volume of the thoracic cavity, increasing the pressure within it. This higher pressure forces air out of the lungs.
The Role of the Diaphragm:
- Inhalation:
The diaphragm contracts, flattening downward. This also increases the volume of the thoracic cavity, creating a negative pressure that draws air into the lungs.
- Exhalation:
The diaphragm relaxes, returning to its dome-shaped position. This decreases the volume of the thoracic cavity, increasing the pressure and forcing air out of the lungs.
In summary:
- Inhalation involves an increase in thoracic volume, leading to a decrease in pressure, which draws air into the lungs.
- Exhalation involves a decrease in thoracic volume, leading to an increase in pressure, which forces air out of the lungs.
The coordinated contraction and relaxation of the ribs, intercostal muscles, and diaphragm are essential for producing these volume and pressure changes, driving the process of breathing.
- Investigate and explain the effect of physical activity on rate and depth of breathing?
The Effect of Physical Activity on Breathing
Physical activity significantly affects both the rate and depth of breathing. As the body’s demand for oxygen increases during exercise, the respiratory system must adjust to meet this heightened need.
Increased Rate of Breathing:
- Increased Oxygen Demand:
When a person engages in physical activity, their muscles require more oxygen to produce energy.
- Increased Respiratory Rate:
To meet this increased oxygen demand, the body increases the rate at which it breathes. This means taking more breaths per minute.
- Enhanced Oxygen Delivery:
By breathing more rapidly, the lungs can deliver more oxygen to the blood, which is then transported to the working muscles.
Increased Depth of Breathing:
- Increased Tidal Volume:
In addition to increasing the rate of breathing, the body also increases the depth of each breath. This means taking larger breaths, inhaling and exhaling more air with each breath.
- Greater Oxygen Uptake:
By taking deeper breaths, the lungs can extract more oxygen from the inhaled air, further enhancing oxygen delivery to the muscles.
- Improved Carbon Dioxide Removal:
Deeper breaths also help to remove carbon dioxide, a waste product of cellular respiration, more efficiently from the body.
Physical activity leads to an increase in both the rate and depth of breathing. This response is essential for meeting the increased oxygen demand of the working muscles and ensuring the efficient removal of carbon dioxide from the body
- Explain the role of goblet cells, ciliated cells and mucus in protecting the gas exchange system from pathogens and particles?
The respiratory system is constantly exposed to a variety of pathogens and particles, such as bacteria, viruses, dust, and pollutants. To protect the delicate gas exchange surfaces of the lungs, the airways are lined with specialized cells and mucus that work together to form a protective barrier.
Goblet Cells:
- Mucus Production:
Goblet cells are specialized epithelial cells that secrete mucus, a sticky substance that lines the airways.
- Trapping Pathogens:
Mucus acts as a sticky trap, capturing pathogens, dust particles, and other foreign substances that enter the airways.
- Moistening Airways:
Mucus also helps to keep the airways moist, preventing them from drying out and becoming irritated.
Ciliated Cells:
- Cilia:
Ciliated cells are epithelial cells that are covered in tiny, hair-like structures called cilia.
- Movement:
The cilia beat in a coordinated manner, propelling the mucus layer, along with trapped pathogens and particles, upward toward the throat.
- Expulsion:
Eventually, the mucus and trapped substances are swallowed or expelled through coughing or sneezing.
Mucus:
- Physical Barrier:
Mucus forms a physical barrier between the airways and the external environment, preventing pathogens from reaching the delicate alveoli.
- Antimicrobial Properties:
Mucus contains antimicrobial substances that can help to kill or neutralize pathogens.
- Moistening:
Mucus helps to keep the airways moist, preventing irritation and damage.
Goblet cells, ciliated cells, and mucus work together to form a protective barrier in the respiratory system. Goblet cells produce mucus, which traps pathogens and particles. Ciliated cells move the mucus layer upward, helping to expel these harmful substances. Mucus also acts as a physical barrier and has antimicrobial properties. This protective mechanism helps to prevent infections and maintain the health of the gas exchange system.